Full-Mouth Dental Implants with Dr. Darren Dickson
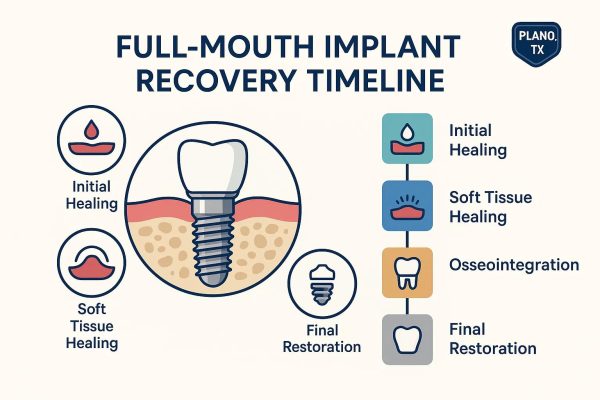
Full-mouth dental implant recovery is a journey from immediate post-surgery healing to the point where your new, stable, implant-supported teeth are fully functional. This guide walks you through what to expect regarding recovery time, the typical healing timeline for dental implants, and how you can best support osseointegration and gum healing after your procedure.
Are you looking for dental implants near you? Trust our implant dentist in Plano, Dr. Darren Dickson, and call our office at(972) 378-9747.
What Are the Key Dental Implant Healing Stages After Surgery?
| Healing Phase | Typical Duration | Expected Symptoms | Recommended Care Actions |
| Initial healing | Days 1–7 | Minor bleeding/spotting, swelling, mild discomfort | Rest, use cold packs, stick to a soft diet, take prescribed pain relief, and avoid forceful rinsing |
| Early soft-tissue healing | Weeks 1–6 | Swelling subsides, gum tissue forms around the implant, slight tenderness | Gentle cleaning, rinse with saline, eat soft foods, avoid smoking |
| Osseointegration | Weeks 6–24 (typically 3–6 months) | Few external symptoms, implant stability gradually improves | Avoid biting down hard on implants, keep the area clean, and attend scheduled X-ray appointments |
| Final restoration | Once osseointegration is confirmed | Minor adjustments to the prosthesis, temporary sensitivity | Getting impressions taken, trying on the prosthesis, gradually increasing chewing force, and regular check-ups |
What Happens During the Initial Healing Stage?
The initial healing stage covers the first 24 to 72 hours and the first week after your surgery. It’s characterized by blood clot formation, localized inflammation, and the beginning of soft-tissue closure. The blood clot protects the surgical site while inflammatory cells work to clear away any debris and prepare the area for new tissue growth, which helps reduce the risk of infection and starts the soft-tissue healing process.
You can typically expect some swelling, bruising, localized pain that usually peaks within 24 to 48 hours, and minor oozing. Your immediate care should involve rest, applying cold compresses in cycles, eating soft foods, and following your medication instructions. We’ll let you know when to change gauze or if you need to contact our dental office for prolonged bleeding. Proper care during this stage helps prevent early complications and sets the stage for smoother osseointegration.
How Does Osseointegration Support Long-Term Implant Stability?
Osseointegration is the biological process where your jawbone grows and integrates directly with the implant surface, creating a strong, stable connection that ensures the implant’s long-term success. Bone formation and remodeling happen over several weeks to months. This process is influenced by factors such as the implant’s surface texture, the quality of your bone, the amount of mechanical force applied, and patient habits like smoking or conditions like diabetes.
Successful osseointegration transforms the initial stability of the implant into a durable biological anchorage. Clinically, this means the implant becomes progressively more stable, which we can measure. Once the stability criteria are met, we can go ahead and place your final restoration. Avoiding inflammation and premature chewing forces during this phase is crucial to prevent fibrous tissue from forming around the implant or the implant failing.
If you have questions or concerns, contact the best dental implant dentist in Plano, Texas, today at (972) 378-9747.
How Can You Effectively Manage Pain and Discomfort After Getting Full-Mouth Dental Implants?
| Option | Onset | Typical Duration | Safety Notes |
| Acetaminophen (OTC) | 30–60 min | 4–6 hours | Safe when dosage limits are followed; minimal stomach upset |
| NSAIDs (e.g., ibuprofen) | 30–60 min | 6–8 hours | Helps reduce inflammation; be mindful of stomach, kidney, and bleeding risks |
| Short-course opioids (prescription) | 15–30 min | Varies | For severe acute pain, use the lowest effective dose for the shortest time |
| Cold therapy | Immediate | First 48–72 hours | Reduces swelling and pain; alternate with rest periods |
Here are the most practical immediate steps for managing pain and swelling:
- Start cold therapy right away: Apply cold packs for 10 to 20 minutes at a time during the first 48 to 72 hours to help minimize swelling.
- Take OTC pain relievers on schedule: Use acetaminophen or NSAIDs as directed to maintain consistent pain control.
- Limit activity and elevate your head: Rest and keep your head higher than your heart can reduce blood flow to the area and ease discomfort.
- Contact us if pain worsens: Reach out to our Plano dental office at (972) 378-9747 if your pain increases after 72 hours or if you develop a fever.

How Can Swelling and Bruising Be Reduced Safely?
Swelling and bruising after getting dental implants are normal inflammatory responses that follow a predictable pattern and can be managed effectively. The initial swelling is due to fluid buildup in the tissues. Applying cold compresses during the first 48 to 72 hours helps constrict blood vessels and reduce swelling. After this initial period, warm compresses can help improve circulation and aid in the resolution of swelling and bruising. You should apply cold compresses in cycles during the first 48 to 72 hours and keep your head elevated, especially when sleeping.
After the first 72 hours, you can transition to warm compresses to help with lymphatic drainage. If you notice persistent swelling on one side, bruising that seems to be getting worse beyond the expected timeframe, or a feeling of fluid under the skin, it could indicate an infection or a hematoma, and you should contact us immediately. Swelling typically decreases gradually over 1 to 2 weeks, and most bruising should resolve within that same period.
How Should Bleeding and Discomfort Be Handled During Recovery?
Some minor oozing and intermittent bleeding are normal right after implant surgery, as your body works to form blood clots and heal the wound. Managing bleeding involves applying gentle pressure, being careful with your mouth, and avoiding activities that increase pressure inside your mouth. Immediately after surgery, apply firm pressure with gauze for 20 to 30 minutes. Avoid spitting and refrain from vigorous rinsing or using straws, as these actions can dislodge clots and increase the risk of bleeding.
If bleeding continues despite pressure, replace the gauze and contact our office for further guidance. Significant or persistent bleeding, or rapidly increasing swelling, requires prompt attention. Pain and discomfort usually respond well to your prescribed pain relievers and local measures. If you experience an unusual increase in pain, develop a fever, or notice any pus, please contact our dentist immediately for an assessment.
What Are the Recommended Aftercare Practices and Lifestyle Adjustments for Full-Mouth Dental Implant Recovery?
Recommended aftercare for full-mouth dental implant recovery focuses on following a diet appropriate for each healing stage, maintaining meticulous yet gentle oral hygiene, gradually resuming activities, and strictly avoiding smoking and alcohol. These practices are crucial for protecting osseointegration and ensuring soft-tissue healing.
What Diet Is Best During Different Recovery Phases?
A phased soft-food diet is essential for tissue repair because it minimizes mechanical stress on the implant sites while ensuring you get the nutrition needed for bone and soft-tissue regeneration. For the first 48 to 72 hours, focus on cool, soft, high-protein liquids and purees. Think smoothies (without a straw), broths, mashed potatoes, and yogurt—these provide the calories and amino acids vital for healing.
Over the first two weeks, you can gradually introduce soft solids like scrambled eggs, oatmeal, and finely ground meats. Continue to avoid hard, crunchy, or very hot foods that could disrupt clots or irritate healing tissues. Key nutrients that support bone healing include adequate protein, calcium, vitamin D, and vitamin C. Consider discussing supplements with your dentist if your dietary intake might be limited. You’ll transition to firmer foods as your comfort level and clinical signs allow, and our dentist will guide you based on your osseointegration progress.
How Should Oral Hygiene Be Maintained Around Dental Implants?
Maintaining oral hygiene around your implants requires a careful balance between controlling plaque and protecting delicate healing tissues. Your approach will evolve from gentle rinses initially to more thorough mechanical cleaning as your tissues mature. For the first 24 hours, avoid rinsing altogether. After that, use saline or a dentist-recommended antiseptic rinse (like a short course of chlorhexidine, if advised) to help reduce bacteria. Gently brushing non-surgical areas and carefully using a soft-bristled toothbrush around the implant sites will help prevent plaque buildup without disturbing sutures or clots.
Once your tissues have healed sufficiently, you can introduce interdental brushes and floss specifically designed for implants to clean around the abutments and prosthesis. Professional teeth cleanings and X-rays are typically scheduled every 3 to 6 months initially. Consistent home care is your best defense against peri-implantitis and is crucial for the long-term success of your implants.
To schedule an appointment at our Plano dental practice, call Dr. Darren Dickson today at (972) 378-9747.

What Activity and Exercise Restrictions Should Be Followed?
Activity restrictions after full-mouth implant surgery are important to prevent increases in blood pressure and mechanical stress that could lead to bleeding, swelling, or implant micromotion during the early healing phases. The safest approach is to prioritize rest for the first 48 to 72 hours. Avoid heavy lifting, strenuous aerobic exercise, and activities that put strain on your head or jaw. Light walking is generally fine and can even help improve circulation. During the first two weeks, you can gradually reintroduce moderate activities, but pay attention to whether you experience increased bleeding or swelling.
You should only return to high-impact or contact sports after receiving clearance from our dentist, which is often after osseointegration is well underway. Activities that significantly raise your blood pressure or involve the Valsalva maneuver (holding your breath and bearing down) should be avoided until your tissues are stable. A gradual, staged return to exercise helps balance your overall health with optimal healing.
Why Is Avoiding Smoking and Alcohol Important for Recovery?
Avoiding smoking and alcohol is critically important because both can negatively impact blood flow, your local immune response, and cellular functions that are essential for osseointegration and soft-tissue healing. Nicotine, found in tobacco products, constricts small blood vessels, reducing the oxygen supply to healing bone and gum tissue. Studies have shown a correlation between smoking and higher rates of implant failure. Alcohol, while sometimes seen as relaxing, can also disrupt the inflammatory process and impair immune function, slowing down tissue repair.
Ideally, you should stop smoking weeks before your surgery and continue to abstain throughout the osseointegration period to maximize your chances of success. Even reducing smoking during this time can improve outcomes. We can discuss smoking cessation strategies with you and may recommend delaying elective implant procedures if significant risk factors are present. Eliminating these habits supports a predictable recovery and ensures your implants last for many years.
What Are the Common Complications of Full-Mouth Dental Implants, and When Should You Seek Help
Common complications include infection, peri-implantitis (inflammation around the implant), nerve injury, sinus perforation (in the upper jaw), and mechanical failure of the implant or prosthesis.
- Key early signs to monitor: Increasing pain after the initial healing period, fever, pus drainage, implant mobility, persistent numbness, or significant changes in your bite.
- Immediate actions: Contact us right away if you suspect an infection or have uncontrolled bleeding. Seek urgent care for worsening nerve symptoms or if you notice exposed hardware.
What Are the Signs of Infection and Implant Failure?
An infection after implant surgery typically shows up as increasing pain after the initial post-operative period, swelling that gets worse instead of better, pus drainage, and systemic symptoms like fever. These signs indicate bacterial colonization that requires prompt medical attention. Implant failure, often due to a lack of osseointegration, may present as persistent implant mobility, bone loss visible on X-rays, and chronic discomfort that lasts beyond the expected healing timeframe, sometimes appearing weeks or months later.
If you suspect an infection, contact our dentist immediately for potential antibiotics, drainage, or cleaning. If mechanical failure is suspected, imaging and possibly implant removal or revision surgery may be necessary. Reporting these issues early and receiving prompt treatment can improve the chances of saving the implant and preventing the infection from spreading.

How Does Bone Grafting Affect Recovery Time and Implant Success?
Bone grafting is used to add bone volume when there isn’t enough natural bone to properly support dental implants, and it typically extends the recovery timeline. This is because the grafted bone needs time to integrate and become strong enough before implants can be placed or loaded. While bone grafting adds time to your overall treatment, often by weeks or months, it significantly improves the long-term success rate for patients with insufficient bone by creating a stable foundation for the implants.
How Does Bone Grafting Influence the Healing Timeline?
Bone grafting typically adds several months to the overall treatment process because the grafted materials need time to develop a blood supply and remodel into your own bone, creating a stable base for implant placement. If implants are placed at the same time as grafting in smaller defects, our dentist might recommend a cautious loading protocol and extended monitoring of osseointegration.
For larger grafts, the standard approach is to place the implants only after the grafted bone has consolidated. Healing times can vary depending on the material used: autografts tend to integrate faster because they contain living cells, while xenografts remodel more slowly but offer long-term volume stability. You should anticipate a longer interval before receiving your final restorations when bone grafting is involved, and your dentist will schedule follow-up imaging and prosthetic placement accordingly.
A New Smile is Closer Than You Think at My Dentist in Plano
Recovering from full-mouth dental implants is a crucial process that significantly impacts your long-term oral health and functionality. By following recommended aftercare practices, you can enhance healing, minimize complications, and ensure the success of your implants. If you’re ready to take the next step towards a healthier smile, contact our implant dentist near you by calling (972) 378-9747 to schedule your tooth replacement consultation.
